title: Unveiling the Origins: Understanding How Colon Cancer Develops
1. Introduction to Colon Cancer: Definition and General Overview
2. Genetic Factors: The Role of Family History and Genetic Mutations
3. Lifestyle and Environmental Influences: Diet, Exercise, and Carcinogens
4. Age and Medical Conditions: How Age and Pre-existing Conditions Contribute
5. Prevention and Early Detection: Strategies to Mitigate Risk
Introduction: Colon cancer, one of the most common types of cancer globally, arises from a complex interplay of genetic, lifestyle, and environmental factors. Understanding how colon cancer develops is crucial for prevention, early detection, and effective treatment. This article delves into the origins of colon cancer, exploring the roles of genetic predispositions, lifestyle choices, and other contributing factors that influence its onset and progression. By unveiling these elements, we aim to provide insights that could lead to more personalized approaches to prevention and management of this serious disease.
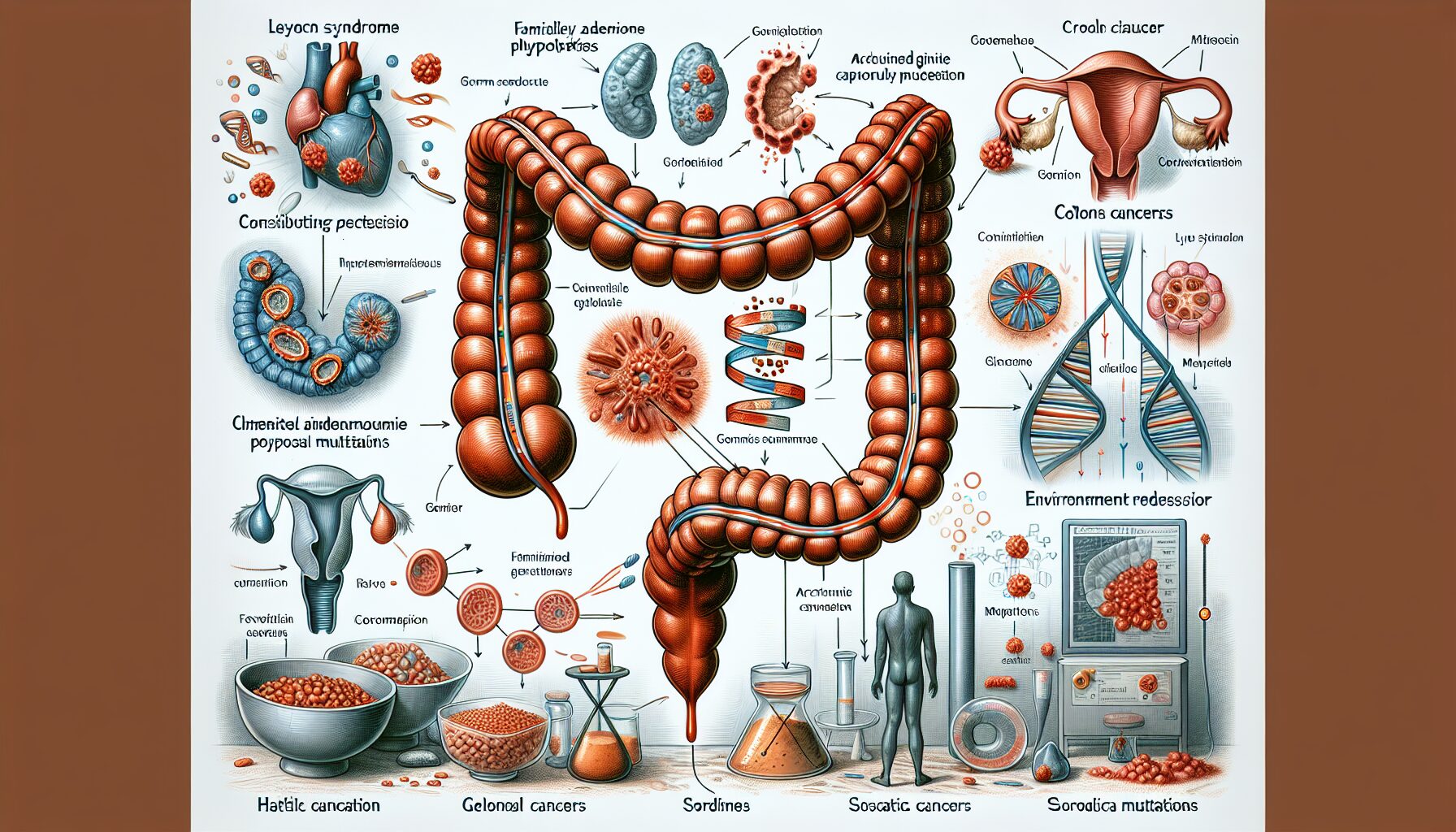
1. Genetic Factors: The Role of Family History and Genetic Mutations
Colon cancer, like many other cancers, is profoundly influenced by genetic factors which play a crucial role in its development. Understanding the genetic underpinnings of colon cancer can provide insights into its mechanisms and potential strategies for prevention and treatment.
Genes are the basic units of heredity in living organisms. They consist of DNA sequences that instruct cells on how to function. In the context of colon cancer, certain genetic mutations—permanent alterations in the DNA sequence of a gene—can lead to abnormal cell growth that may evolve into cancer. These mutations can be inherited (germline) or acquired (somatic). Germline mutations are present from birth and are passed from parent to child, affecting every cell in the body. Conversely, somatic mutations occur at some point during a person’s life and are not inherited but rather arise from factors like environmental exposure or errors in DNA replication.
One of the most significant inherited syndromes linked to an increased risk of developing colon cancer is Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC). Individuals with Lynch syndrome have mutations in mismatch repair (MMR) genes, which are crucial for correcting DNA replication errors. This predisposition can lead to microsatellite instability—a type of genetic hypermutability—which increases the risk of cancer development. Approximately 3% to 5% of all cases of colon cancer are associated with Lynch syndrome.
Another genetic condition strongly linked to colon cancer is familial adenomatous polyposis (FAP), an autosomal dominant disorder characterized by the early onset of hundreds to thousands of polyps in the colon and rectum during the teenage years. These polyps, though initially benign, have a high probability of becoming malignant if left untreated. FAP is caused by mutations in the APC gene, a critical regulator of cell growth and apoptosis (programmed cell death).
Besides these hereditary syndromes, individual genetic mutations can also influence the risk of sporadic (non-hereditary) colon cancers. For example, mutations in the APC gene, KRAS gene, and P53 tumor suppressor gene have been implicated in the pathogenesis of sporadic colon cancers. The APC gene mutation is particularly notable because it is seen in about 80% of all sporadic cases. The mutation leads to abnormal accumulation of β-catenin—a protein involved in regulating cell adhesion and gene transcription—thus promoting uncontrolled cell division.
Moreover, recent advances in genomic medicine have allowed researchers to identify numerous other genes that may contribute to increased susceptibility to colon cancer. For instance, variations in genes like SMAD7, which plays a role in signaling pathways that control cell proliferation, have been associated with a modestly increased risk of colon cancer.
In conclusion, both inherited and acquired genetic factors play significant roles in the development of colon cancer. While inherited conditions like Lynch syndrome and FAP account for a small percentage of all cases, they provide essential clues about the molecular pathways involved in cancer development. Similarly, understanding somatic mutations helps explain how external factors and internal processes can lead to cancer later in life.
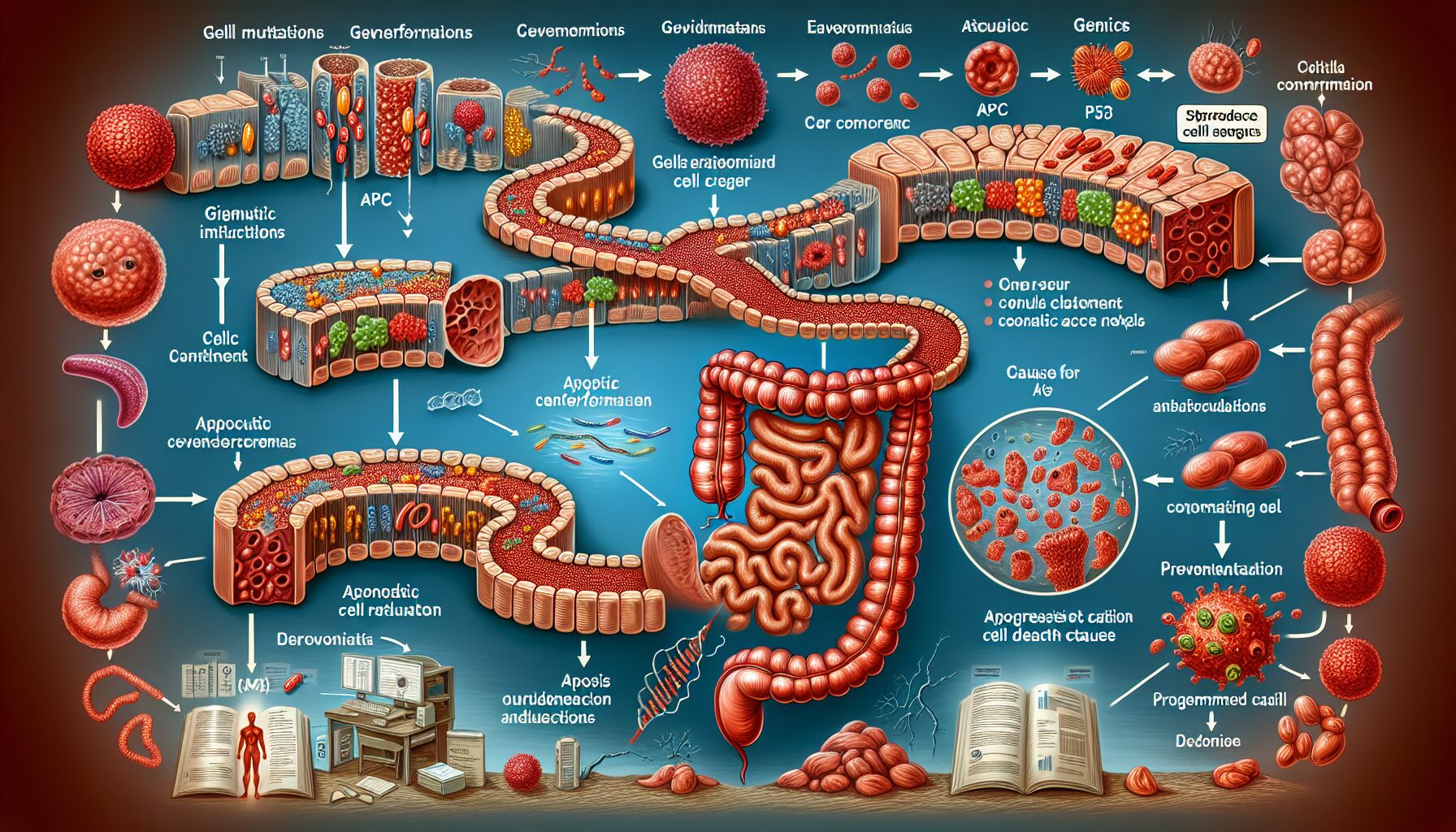
2. Genetic Factors: The Role of Family History and Genetic Mutations
Understanding the genetic underpinnings of colon cancer is crucial for both prevention and treatment. Colon cancer, like many other cancers, can be significantly influenced by both inherited genetic factors and acquired mutations in the DNA of colon cells. Genetic predisposition to colon cancer means that the disease may be passed down through family generations, making family history a vital component in assessing risk.
The role of family history in colon cancer cannot be understated. Approximately 20-25% of patients with colon cancer have a family history of the disease, suggesting a strong genetic component. This familial risk increases if more than one first-degree relative (parent, sibling, or child) has been diagnosed with colon or rectal cancer, especially if the cancer was diagnosed at a young age. Individuals with a family history of colon cancer are often advised to undergo earlier and more frequent screening procedures, such as colonoscopies, to catch potential malignancies at their earliest, most treatable stages.
In addition to family history, specific genetic mutations play a critical role in the development of colon cancer. One of the most well-known genetic factors associated with an increased risk of developing colon cancer is hereditary nonpolyposis colorectal cancer (HNPCC), also known as Lynch syndrome. Lynch syndrome is caused by mutations in mismatch repair (MMR) genes which are crucial for correcting DNA replication errors. People with Lynch syndrome have an 80% lifetime risk of developing colorectal cancer due to these genetic defects.
Another significant genetic condition linked to increased colon cancer risk is familial adenomatous polyposis (FAP). This condition is characterized by the early onset of hundreds to thousands of polyps in the colon and rectum during the teenage years. These polyps, although initially benign, have a high likelihood of becoming malignant if not removed. FAP is caused by mutations in the APC gene, which normally helps control cell growth and death.
Beyond these hereditary conditions, sporadic (non-hereditary) mutations can also lead to colon cancer. These mutations often occur from environmental factors or as a result of aging. For example, mutations in the adenomatous polyposis coli (APC) gene can spontaneously occur without any familial predisposition. The APC gene acts as a tumor suppressor gene, and its inactivation is considered one of the earliest steps in most cases of colon cancer development.
Moreover, the mutation of oncogenes such as KRAS plays a pivotal role in the progression of many colorectal cancers. KRAS mutations are involved in about 40% of all colorectal cancers and contribute to uncontrolled cell division and tumor growth.
In conclusion, both inherited genetic factors and acquired mutations significantly influence the risk and development of colon cancer. Understanding these genetic influences not only helps in assessing individual risk but also assists in developing targeted therapies that address specific genetic abnormalities present in tumors. As research continues to evolve, genetic testing and personalized medicine are becoming increasingly important tools in the fight against colon cancer, offering hope for more effective prevention and treatment strategies tailored to each patient’s unique genetic profile.
3. Lifestyle and Environmental Influences: Diet, Exercise, and Carcinogens
The development of colon cancer is significantly influenced by lifestyle and environmental factors. These elements can either increase the risk or provide some degree of protection against the disease. Among the most impactful are diet, exercise, and exposure to carcinogens.
Diet plays a crucial role in colon cancer development. High consumption of red and processed meats has been linked to an increased risk of colon cancer. These foods are high in fats and often contain compounds that, when digested, can lead to the formation of cancer-causing chemicals. Conversely, diets rich in fruits, vegetables, and whole grains have been shown to reduce the risk. These foods contain a variety of vitamins, minerals, fibers, and antioxidants that help protect against cancer. Fiber, for example, helps to keep the digestive system healthy and can prevent harmful substances in the diet from affecting the cells lining the colon.
Exercise is another critical factor in mitigating the risk of colon cancer. Regular physical activity helps to maintain a healthy body weight, which is important because obesity is a significant risk factor for many forms of cancer, including colon cancer. Exercise also promotes healthy digestion and can reduce inflammation in the body. Studies have consistently shown that individuals who engage in regular physical activity have a lower incidence of colon cancer compared to those who are sedentary.
Carcinogens in the environment are also potential risk factors for colon cancer. These can include chemicals found in tobacco smoke, air pollution, and certain types of industrial chemicals. For instance, asbestos, which is known for causing lung cancer, has also been linked to an increased risk of colon cancer when ingested. Additionally, exposure to large amounts of radiation or certain chemicals like benzene can damage the DNA in cells of the colon, leading to cancer.
The interaction between diet, exercise, and carcinogen exposure can significantly alter an individual’s risk profile for colon cancer. For instance, a person who eats a diet high in processed meats and low in fiber-rich foods might increase their risk more significantly if they also smoke or are exposed to other environmental carcinogens. On the other hand, regular exercise and a healthy diet can help mitigate some of the risks associated with environmental carcinogens.
Understanding these lifestyle and environmental factors provides a clear pathway for individuals to modify their habits in ways that could potentially lower their risk of developing colon cancer. It highlights the importance not only of what we eat but how we live our lives more broadly—including our physical activity levels and our exposures to various environmental risks. By making informed choices about diet, exercise, and exposure to carcinogens, individuals can actively participate in reducing their risk of this serious disease.
4. Age and Medical Conditions: How Age and Pre-existing Conditions Contribute
The link between age, pre-existing medical conditions, and the development of colon cancer is a critical area of study in understanding the disease’s etiology. As individuals age, the risk of developing colon cancer increases significantly. Statistics show that over 90% of people diagnosed with colon cancer are aged 50 or older. This is largely due to the cumulative effects of cellular damage over time, which can lead to the mutations that cause cancer.
Aging cells are more susceptible to genetic mutations because the mechanisms that repair DNA and control cell division become less effective. As a person ages, these cellular processes continue to degrade, increasing the likelihood of abnormal cell growth. Furthermore, the immune system, which plays a role in detecting and destroying abnormal cells, also weakens with age, reducing its ability to combat early forms of cancer.
In addition to age, certain pre-existing medical conditions can also heighten the risk of developing colon cancer. One such condition is chronic inflammatory diseases of the colon such as Crohn’s disease and ulcerative colitis. These conditions cause continuous inflammation of the colon, which can lead to changes in the DNA of cells in the colon lining. Over time, these genetic changes can accumulate and increase the risk of colon cancer.
Another significant pre-existing condition linked to increased risk of colon cancer is diabetes, particularly type 2 diabetes. Research indicates that individuals with type 2 diabetes have a 30% higher risk of developing colon cancer than those without diabetes. The link between diabetes and increased colon cancer risk is thought to be due to excess insulin or insulin-related growth factors that promote tumor growth.
Obesity is another condition that significantly affects colon cancer risk. Excess body fat has been associated with increased levels of inflammation and higher concentrations of certain hormones, like insulin, which can promote cancer growth. Furthermore, fatty tissue produces adipokines – proteins that can cause chronic inflammation and are believed to contribute to cancer development.
Additionally, a history of adenomatous polyps (adenomas), which are benign tumors found in the colon or rectum, greatly increases the risk of developing into colon cancer if not removed. Adenomas are considered precancerous conditions and are an important focus for early detection strategies in preventing colon cancer.
Understanding how age and medical conditions contribute to the development of colon attack underscores the importance of regular screenings and monitoring for those at increased risk. For older adults and individuals with these pre-existing conditions, regular colonoscopies can detect precancerous polyps before they turn into malignant tumors. Moreover, managing chronic conditions like diabetes and maintaining a healthy weight through diet and exercise are crucial preventative measures that can help reduce the risk of developing colon cancer.
In conclusion, while age is an uncontrollable factor, awareness and management of pre-existing medical conditions can play a significant role in reducing one’s risk of developing colon cancer. It highlights the need for targeted prevention strategies that consider both age and individual health histories in their approach.
5. Prevention and Early Detection: Strategies to Mitigate Risk
Colon cancer, like many other forms of cancer, can often be prevented through the implementation of effective strategies aimed at mitigating risk factors and enhancing early detection. Understanding and applying these strategies can significantly reduce the incidence of this disease, potentially saving countless lives.
Dietary Modifications: One of the most impactful prevention strategies is dietary modification. Diets high in red and processed meats have been linked to an increased risk of colon cancer. Conversely, diets rich in fruits, vegetables, and whole grains provide protective benefits due to their high fiber content and the presence of cancer-fighting antioxidants. Incorporating such foods into daily meals can help reduce the risk of colon cancer.
Regular Exercise: Physical activity is another crucial preventive measure. Regular exercise helps maintain a healthy weight, which is important because obesity is a significant risk factor for colon cancer. Additionally, exercise promotes healthy digestion and can reduce the time that the colon is exposed to harmful substances in waste, thus potentially reducing the risk of cancer development.
Avoiding Tobacco and Limiting Alcohol Consumption: Smoking is a well-known risk factor for many types of cancer, including colon cancer. Quitting smoking can markedly decrease one’s risk. Similarly, excessive alcohol consumption has been linked to an increased risk of colon cancer. Limiting alcohol intake to moderate levels is advised as part of a comprehensive prevention strategy.
Regular Screening Tests: Early detection through screening is paramount in preventing colon cancer or catching it in its early stages when it is most treatable. Screening methods such as colonoscopies allow healthcare providers to detect precancerous polyps and remove them before they turn into cancer. The American Cancer Society recommends that individuals at average risk of colon cancer begin regular screenings at age 45. However, those with additional risk factors, such as a family history of the disease, may need to start earlier.
Awareness of Family History: Since genetic factors can play a significant role in the development of colon cancer, being aware of one’s family history is essential. Individuals with a strong family history may require genetic counseling and earlier or more frequent screening tests. This proactive approach allows for early intervention and increased surveillance, substantially lowering the risk of developing colon cancer.
Use of Aspirin: Some studies suggest that the use of aspirin may reduce the risk of developing colon cancer due to its anti-inflammatory properties. However, because aspirin can also cause gastrointestinal bleeding and other side effects, it should only be used for this purpose under the guidance of a healthcare provider.
Maintaining a Healthy Gut Microbiome: Emerging research indicates that a healthy gut microbiome may play a role in preventing colon cancer. Diets high in fiber support a diverse and balanced microbiome, which can positively impact overall colon health.
Implementing these strategies requires both individual actions and public health initiatives to increase awareness and accessibility of preventive measures. By adopting these lifestyle changes and adhering to recommended screening guidelines, individuals can significantly decrease their risk of developing colon cancer, highlighting the power of prevention and early detection in combating this disease.
Conclusion:
The development of colon cancer is a multifaceted process influenced by genetics, age, lifestyle choices, and environmental exposures. Recognizing the complexity of these factors offers valuable perspectives on prevention strategies and early detection methods that can significantly reduce the risk or aid in managing the disease effectively. It underscores the importance of personalized medical approaches based on individual risk profiles, family history, and lifestyle factors. Ultimately, increased awareness and proactive management are key in reducing the incidence and impact of colon cancer, making it essential for individuals to engage actively with healthcare providers in adopting preventive measures tailored to their specific needs.
