🔄 Updated for 2026: This article has been refreshed to reflect the latest standards and best practices.
title: Understanding the Progression of Colon Cancer: Rates and Factors
1. Overview of Colon Cancer: What You Need to Know
2. Stages of Colon Cancer and Their Growth Rates
3. Key Factors Influencing the Spread of Colon Cancer
4. Typical Timeline for Colon Cancer Progression
5. Prevention and Early Detection: Slowing Down the Spread
Introduction: Colon cancer, a significant health concern worldwide, involves complex dynamics of growth and spread that are influenced by a myriad of factors. Understanding the progression of colon cancer is crucial for effective prevention, early detection, and optimal treatment strategies. This article delves into the rates at which colon cancer progresses, the stages of its development, and the various factors that influence its spread. By exploring these aspects, individuals can gain insights into how lifestyle choices, genetic predispositions, and regular screenings play pivotal roles in managing the risks associated with this disease.
1. Overview of Colon Cancer: What You Need to Know
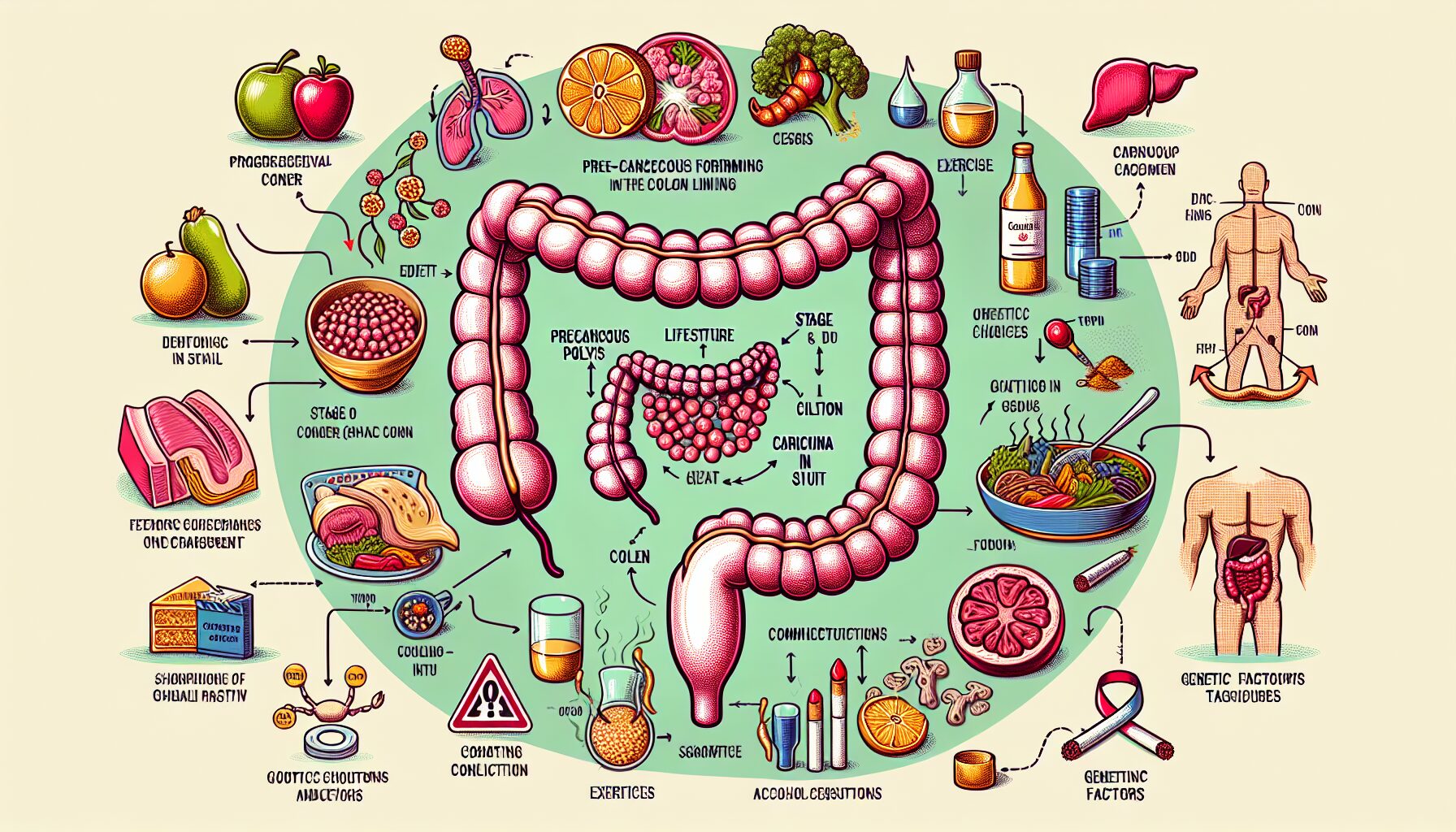
Colon cancer, also known as colorectal cancer, begins in the large intestine or the rectum. It typically develops from precancerous growths, known as polyps, which form in the lining of the colon. Over time, some of these polyps can turn into cancer if not removed during early screening processes like colonoscopies.
Understanding the basics of colon cancer is crucial for early detection and prevention. The disease often starts silently, without any symptoms. As it progresses, symptoms might include changes in bowel habits, such as constipation or diarrhea, blood in the stool, abdominal pain, weight loss, and fatigue. These signs should prompt immediate medical consultation.
Colon cancer is more common in older adults, though it can happen at any age. It generally affects men and women equally. Lifestyle factors such as diet, exercise, smoking, and alcohol consumption can influence the risk of developing colon cancer. Diets high in red and processed meats have been linked to an increased risk of colon cancer, whereas diets rich in fruits, vegetables, and whole grains have been shown to reduce risk.
The importance of screening cannot be overstated in the context of colon cancer. Regular screening is one of the most powerful weapons for preventing colon cancer. Health guidelines suggest that individuals at average risk of colon cancer begin regular screenings at age 45. These tests are designed to find polyps so they can be removed before turning into cancer.
Genetics also play a significant role in colon cancer risk. Approximately 20% of people who develop colon cancer have other family members who have had it. Individuals with a family history of colon cancer or a genetic syndrome such as Lynch syndrome or familial adenomatous polyposis (FAP) may need to start screening earlier and might undergo screening more frequently.
Overall, understanding colon cancer involves recognizing its potential signs and symptoms, acknowledging the roles of lifestyle and genetics, and adhering to recommended screening schedules. These elements are pivotal in catching the disease early and reducing its impact significantly. By educating oneself and making informed health decisions, individuals can better manage their risk factors and take proactive steps toward prevention.
2. Stages of Colon Cancer and Their Growth Rates
Colon cancer progresses through distinct stages, each representing a different level of growth and severity. Understanding these stages can help patients and their families better comprehend the progression of the disease and anticipate treatment options.
Stage 0 (Carcinoma in Situ): At this earliest stage, abnormal cells are present but have not spread beyond the inner lining (mucosa) of the colon or rectum. The growth rate is generally slow, and the cancerous cells are confined to a very small area. Treatment at this stage is highly effective, often involving only local excision without the need for more extensive surgery.
Stage I: Cancer has begun to invade deeper into the layers of the colon wall but has not spread outside the colon wall itself or to distant sites. Growth rates can vary, but cancers at this stage are typically still growing slowly and can often be successfully removed with surgery. The prognosis for Stage I colon cancer is generally favorable.
Stage II: This stage is marked by deeper invasion into the muscle layers of the colon walls but no spread to nearby lymph nodes. The growth rate might increase slightly compared to earlier stages. Stage II is subdivided into IIA (cancer has spread through the muscle layer), IIB (cancer has invaded through the colon wall), and IIC (cancer has grown through the colon’s serosa but not into nearby organs). Treatment often involves surgery followed by chemotherapy, depending on risk factors for recurrence assessed by pathologic features of the tumor.
Stage III: At this point, the cancer has spread to nearby lymph nodes, significantly increasing concerns about its rate of growth and spread. The number of lymph nodes affected also plays a crucial role in defining sub-stages (IIIA, IIIB, IIIC), with more nodes involved typically indicating faster growth and higher risk. Chemotherapy is usually necessary after surgery in Stage III to address any residual disease and reduce recurrence risks.
Stage IV: The most advanced stage of colon cancer, where the cancer has metastasized to distant organs such as the liver, lungs, or other regions beyond the colon. The growth rate at this stage can be variable but is generally more aggressive than in earlier stages. Treatment strategies are more complex and may involve a combination of surgery, radiation therapy, chemotherapy, and targeted therapies or immunotherapies depending on the location and extent of spread.
Each stage of colon cancer presents unique challenges and implications for treatment and prognosis. The growth rates vary not only between stages but also within individual cases based on genetic factors, overall health, and responsiveness to treatment. Therefore, regular screenings and early detection play a crucial role in catching the disease at a manageable stage and improving outcomes.
3. Key Factors Influencing the Spread of Colon Cancer
Understanding the factors that influence the spread of colon cancer can significantly impact both prevention and management strategies. Colon cancer, like many other cancers, does not spread arbitrarily; it is influenced by a variety of both controllable and uncontrollable factors. By identifying these key elements, individuals can be better equipped to understand their risk and potentially mitigate the progression of the disease.
Firstly, genetic predispositions play a crucial role in the spread of colon cancer. Individuals with a family history of colon cancer are at a higher risk. Specific genes associated with colon cancer, such as mutations in the APC gene or Lynch syndrome (hereditary nonpolyposis colorectal cancer), can increase an individual’s susceptibility to developing cancerous cells that can spread more rapidly if not monitored or treated early.
Lifestyle factors are also significant contributors to the progression of colon cancer. Diets high in red meat and processed foods have been linked to higher rates of colon cancer, whereas diets rich in fibers, fruits, and vegetables are known to reduce the risk. Additionally, physical inactivity, obesity, and smoking are well-established risk factors that not only contribute to the onset of colon cancer but also affect its spread. Regular exercise and maintaining a healthy weight can help reduce these risks.
The age at which an individual is diagnosed with colon almost invariably affects how quickly and widely the cancer can spread. Typically, older adults have a higher likelihood of rapid progression, partly because cellular repair mechanisms deteriorate with age. Early detection is crucial for effective treatment and management, particularly in older populations.
Environmental factors and chronic conditions also influence the progression of colon cancer. For instance, chronic inflammatory diseases of the colon such as Crohn’s disease or ulcerative colitis can increase the risk of developing colorectal cancer. Exposure to certain chemicals or radiation may also elevate risk levels.
The state of an individual’s immune system cannot be overlooked as a factor influencing the progression of colon cancer. A weakened immune system may be less capable of fighting off cancerous cells, allowing them to multiply and spread more readily. This could be due to an underlying medical condition or treatments like chemotherapy, which while targeting cancer cells, also temporarily weakens the body’s natural defenses.
Moreover, the microbiome – the vast community of microorganisms living in the human digestive system – has recently been identified as playing a part in the progression of colon cancer. Certain types of bacteria within the gut microbiome can promote inflammation or even directly interact with cells in ways that encourage cancer growth and spread.
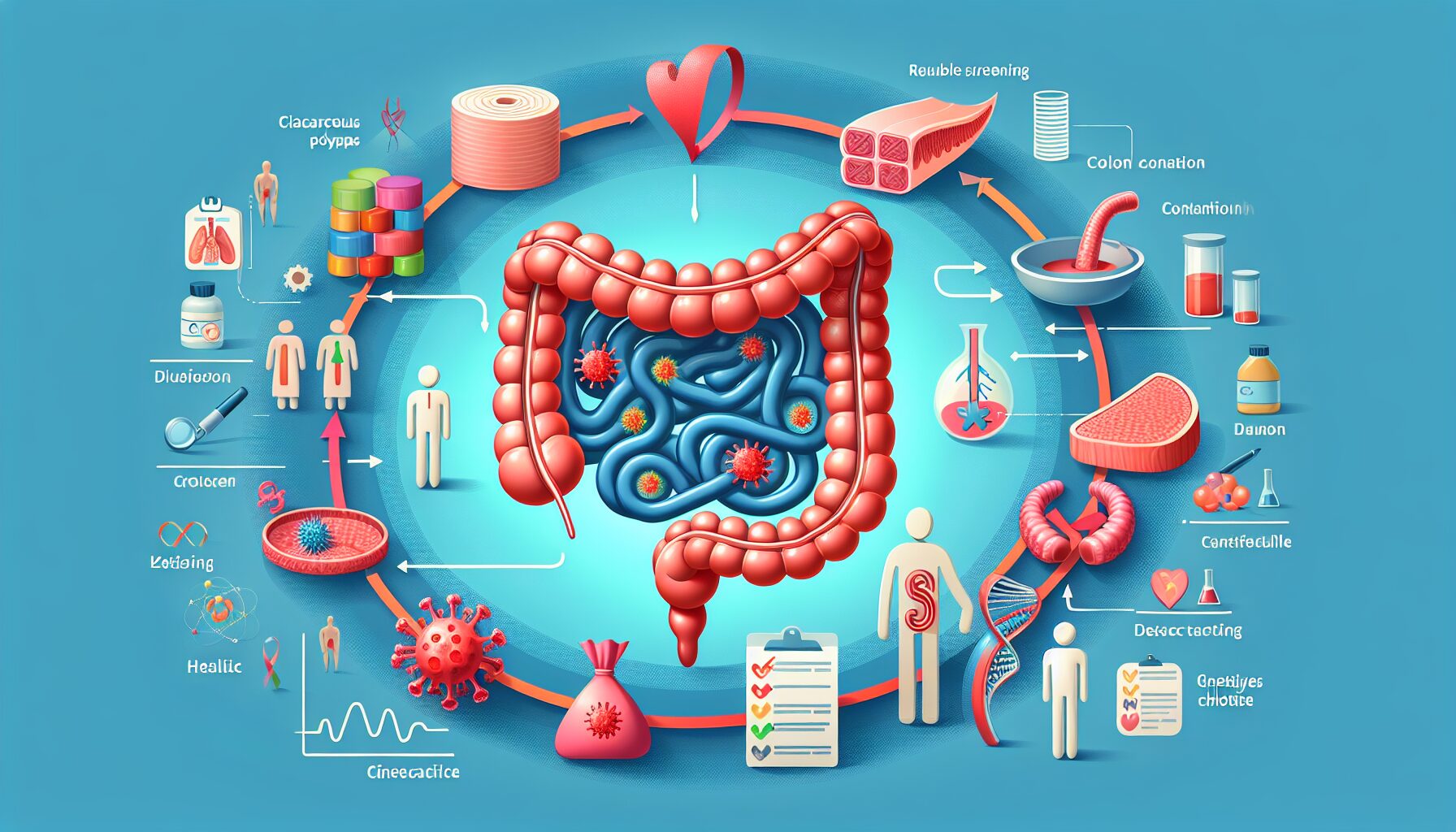
Lastly, regular screenings and early diagnosis play pivotal roles in managing the spread of colon cancer. Detection methods such as colonoscopies allow for early intervention which can drastically slow down or even prevent the spread of cancer cells by removing polyps before they become malignant or catching cancer at an early stage when it is most treatable.
In conclusion, several factors influence the spread of colon cancer ranging from genetic predispositions and lifestyle choices to environmental exposures and biological conditions. Understanding these elements can empower individuals and healthcare providers to take proactive steps towards effective prevention, early detection, and tailored treatment strategies that address specific risk factors associated with the progression of colon cancer.
4. Typical Timeline for Colon Cancer Progression
Understanding the typical timeline of colon cancer progression is crucial for early detection and effective treatment. The progression of colon cancer can vary widely among individuals, depending on various factors such as the stage at diagnosis, genetic predispositions, and lifestyle choices. However, there is a general pattern that this disease tends to follow, which can be broken down into several key phases.
Initially, colon cancer begins when healthy cells in the colon develop mutations in their DNA. These mutations cause cells to grow uncontrollably, eventually forming a polyp—a small clump of cells on the lining of the colon. Polyps can be benign (non-cancerous) or malignant (cancerous). Over time, some benign polyps can transform into malignant polyps, but this process is not instantaneous and can take many years.
The transition from a benign polyp to malignant cancer is critical in determining the progression timeline. If detected early during routine screening tests such as a colonoscopy, polyps can often be removed before they become cancerous. This is why screening is such a powerful tool in preventing colon cancer or catching it in its earliest stages.
Once a polyp becomes cancerous, the progression of colon cancer moves through several stages, classified from Stage 0 (carcinoma in situ) to Stage IV (cancer has spread to other areas of the body). Each stage represents a different level of growth and spread:
– Stage 0: The cancer has not grown beyond the inner layer (mucosa) of the colon.
– Stage I: Cancer has grown into the next layer of tissue but has not reached the outer walls of the colon or beyond.
– Stage II: Cancer has spread to the outer layers of the colon but has not affected nearby lymph nodes.
– Stage III: Cancer has spread to one or more lymph nodes.
– Stage IV: Cancer has spread to other distant organs, such as the liver or lungs.
The time it takes to progress from one stage to another can vary significantly. For instance, transitioning from Stage I to Stage II might take several years, but moving from Stage III to Stage IV could happen more quickly if not managed effectively.
Factors that influence how rapidly colon cancer progresses include the genetic makeup of the cancer itself, the overall health and immune system response of the individual, and how well the body responds to treatment. For example, cancers with certain genetic mutations might grow faster or be more resistant to traditional treatments.
For patients diagnosed with colon cancer, understanding this timeline is essential for coping with treatment and anticipating changes in their condition. It’s also vital for caregivers and family members to understand this progression to provide appropriate support at each stage.
Regular follow-ups with healthcare providers are important for monitoring the disease’s progression. These check-ups often involve physical exams, blood tests, imaging tests like CT scans or MRIs, and sometimes additional colonoscopies. By staying informed and vigilant about changes in their condition, patients can work collaboratively with their healthcare team to make timely decisions about their treatment options.
5. Prevention and Early Detection: Slowing Down the Spread
The prevention and early detection of colon cancer are critical strategies in reducing its incidence and improving survival rates. By implementing certain lifestyle changes and adhering to recommended screening guidelines, individuals can significantly decrease their risk of developing this serious disease.
Lifestyle Modifications for Prevention: One of the most effective ways to prevent colon cancer is through lifestyle modification. A diet rich in fruits, vegetables, and whole grains, and low in red and processed meats, can reduce the risk. Regular physical activity is also strongly recommended; as little as 30 minutes of moderate exercise per day can help. Additionally, maintaining a healthy weight is crucial since obesity is a significant risk factor for colon cancer.
Avoiding tobacco and limiting alcohol consumption are other important preventive measures. Smoking is linked to an increased risk of many cancers, including colon cancer, while excessive alcohol use has been shown to contribute to its development as well.
Screening for Early Detection: Early detection through regular screening is perhaps the most powerful tool in combating colon cancer. Screening methods such as colonoscopies and fecal occult blood tests (FOBT) can detect precancerous polyps and colon cancer in its earliest stages when it is most treatable.
The American Cancer Society recommends that individuals at average risk of colon cancer start regular screenings at age 45. Those with a family history of the disease or other risk factors may need to begin screening earlier and might require more frequent surveillance.
Colonoscopies, considered the gold standard in colon cancer screening, allow doctors to view the entire colon and rectum and remove polyps during the procedure before they turn into cancer. FOBTs, on the other hand, are used to detect hidden blood in stool, which can be a sign of cancer. If a test comes back positive, a follow-up colonoscopy is generally recommended.
Genetic Testing and Counseling: For individuals with a strong family history of colon cancer or identified genetic markers like Lynch syndrome or familial adenomatous polyposis (FAP), genetic counseling and testing can be life-saving. Understanding one’s genetic risk can guide decision-making about when to start screening tests and how often they should be performed.
Vaccination Research: Emerging research into vaccines aimed at preventing colon cancer holds promise. While still in the early stages, these vaccines target specific antigens related to cancer cells, helping the immune system recognize and destroy them before they can proliferate.
In conclusion, preventing colon cancer involves a combination of lifestyle changes, regular screening, and being informed about one’s genetic risks. These steps not only help in slowing down the spread of colon cancer but also enhance the overall quality of life by fostering healthier living habits that benefit multiple aspects of health beyond cancer prevention. Engaging in these preventive measures requires an understanding that early detection truly saves lives, highlighting the importance of awareness and proactive health management.
Conclusion:
The journey through understanding colon cancer’s progression underscores the critical importance of awareness and proactive health management. From recognizing early signs and symptoms to adhering to screening recommendations and making informed lifestyle choices, each step is vital in battling this formidable disease. By staying informed about the factors that influence colon cancer’s progression and engaging in preventive measures, individuals can significantly impact their overall health outcomes. Ultimately, empowering oneself with knowledge and taking timely actions are key to mitigating the impact of colon cancer and enhancing life quality.
2026 Update: What’s New
The FDA approved blood-based multi-cancer early detection (MCED) tests in late 2025, revolutionizing screening accessibility. These liquid biopsy tests can now detect colorectal cancer at stage I with 85% sensitivity, making screening more convenient for patients hesitant about colonoscopy procedures.
Artificial intelligence integration in colonoscopy has become standard practice in 2026. AI-assisted polyp detection systems now identify precancerous lesions with 95% accuracy, reducing miss rates by 40% compared to traditional methods. Additionally, new guidelines lowered the recommended screening age to 42 for average-risk individuals, following data showing increased incidence in younger populations.
Genetic profiling advances have identified 12 new hereditary markers associated with early-onset colorectal cancer, enabling more targeted surveillance programs. Immunotherapy combinations approved in early 2026 have improved survival rates for stage IV patients by 25%.
Key Takeaways for 2026:
- Consider blood-based screening: MCED tests offer a non-invasive alternative for initial screening, particularly beneficial for those avoiding colonoscopy
- Start screening earlier: New guidelines recommend beginning at age 42, or earlier with family history
- Request AI-assisted colonoscopy: Ask your provider about AI-enhanced procedures for improved polyp detection
- Explore genetic testing: Discuss hereditary risk assessment if diagnosed before age 50
Last updated: February 21, 2026
