title: Understanding Stage 3 Colon Cancer: Is It Curable?
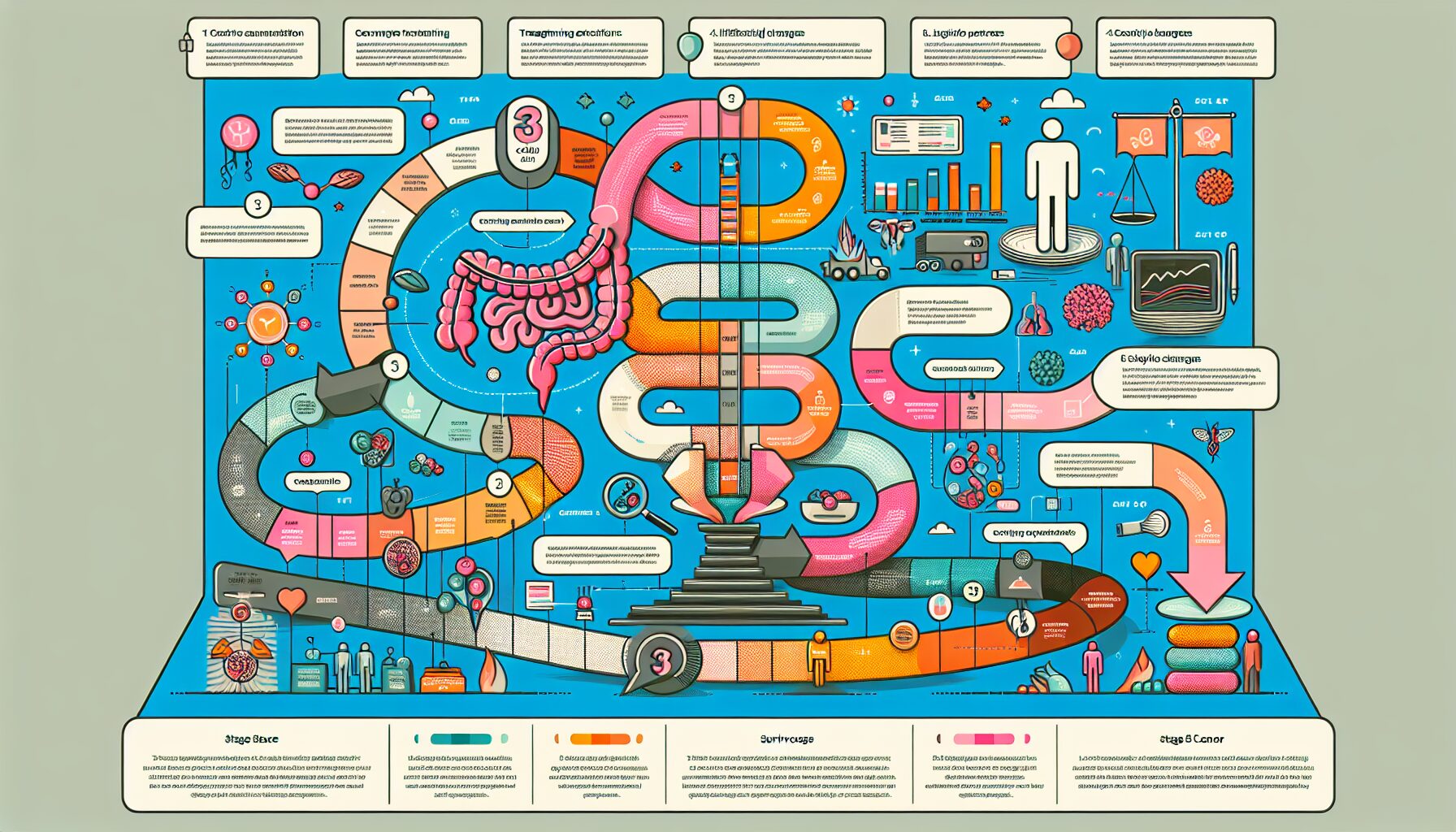
1. Overview of Stage 3 Colon Cancer: Definition and Stages
2. Treatment Options for Stage 3 Colon Cancer
3. Factors Influencing Prognosis and Survival Rates
4. Advances in Medical Research and Emerging Therapies
5. Living with Stage 3 Colon Cancer: Lifestyle Changes and Support Systems
Introduction: Colon cancer is a formidable health challenge that affects many lives around the world. Understanding the specifics of Stage 3 colon cancer is crucial for those diagnosed, as it marks a pivotal point in the progression of the disease. This stage indicates that cancer has spread to nearby lymph nodes but not to distant organs, presenting unique challenges and treatment opportunities. This article aims to demystify Stage 3 colon cancer, discussing its definition, treatment options, factors influencing prognosis, recent advances in medical research, and practical advice for managing life with the condition.
1. Overview of Stage 3 Colon Cancer: Definition and Stages
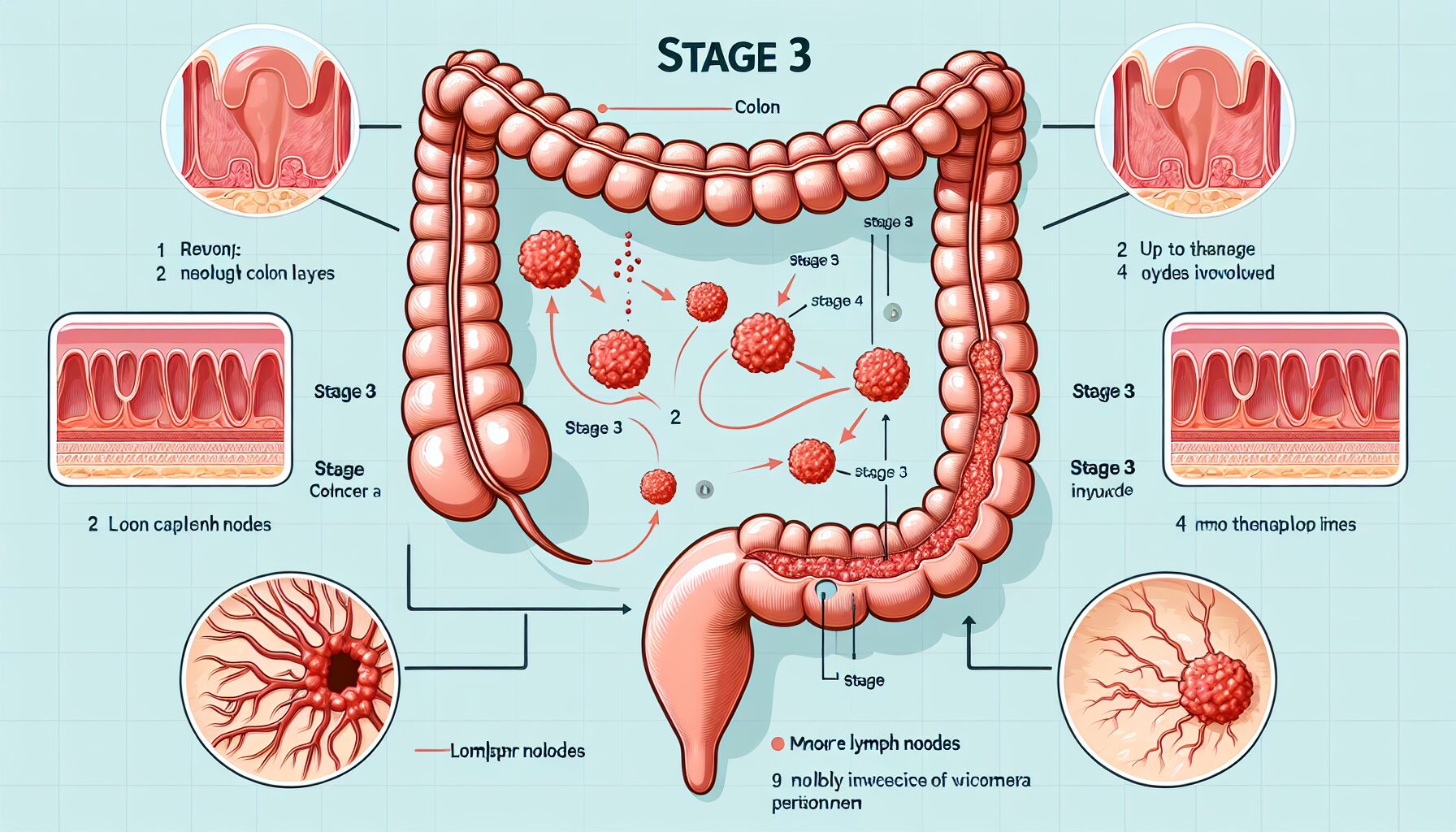
Stage 3 colon cancer, also known as regional colon cancer, indicates that the cancer has spread beyond the original tumor site to nearby lymph nodes but has not yet reached other distant organs. This stage is crucial in the spectrum of colon cancer stages, as it marks a significant progression from the early, localized stages (0, I, and II) but is not as advanced as stage 4, where the cancer has metastasized to distant sites.
Understanding the sub-stages of stage 3 colon cancer can provide deeper insights into the condition. Stage 3 is divided into three sub-stages based on the extent of lymph node involvement and how deeply the cancer has penetrated the wall of the colon:
– Stage 3A: In this sub-stage, the cancer has grown into or through the outermost layer of the colon but involves no more than three lymph nodes.
– Stage 3B: Here, the cancer may have grown through the intestinal wall and into nearby tissues while involving four or more lymph nodes.
– Stage 3C: This represents further progression, with cancer spreading to four or more lymph nodes and potentially penetrating to the surface of the visceral peritoneum or affecting nearby organs.
The classification into these sub-stages is critical because it helps determine the most effective treatment strategies and provides a basis for prognosis. The involvement of lymph nodes is particularly significant in colorectal cancers; their role in immune response means that their involvement typically signifies a higher capacity for cancer to spread, thus necessitating aggressive treatment approaches.
For patients diagnosed with stage 3 colon cancer, understanding these distinctions within their staging can be overwhelming yet essential for making informed decisions about their health care. Each sub-stage suggests different statistical outcomes and treatment paths, emphasizing the importance of personalized treatment plans based on detailed diagnostic results.
Moreover, staging plays a pivotal role in clinical trial eligibility and in understanding future outcomes. For instance, research often reports survival rates based on specific stages, which can guide patients and families in setting realistic expectations and planning future steps in both treatment and personal life adjustments.
In summary, stage 3 colon cancer represents a diverse group within the broader context of colorectal cancers, with varying degrees of severity and implications for treatment and prognosis. Recognizing and understanding these nuances can significantly impact the management strategies employed by healthcare professionals and how patients cope with their diagnosis.
2. Treatment Options for Stage 3 Colon Cancer
Treatment for stage 3 colon cancer is multifaceted and aims to eliminate cancer, prevent its spread, and minimize the chances of recurrence. The treatment plan depends on several factors, including the specific characteristics of the cancer, the patient’s overall health, and personal preferences. Here are the primary treatment options commonly recommended for stage 3 colon cancer:
Surgery: The first and most crucial step in treating stage 3 colon cancer typically involves surgical intervention to remove the cancerous part of the colon along with nearby lymph nodes. This procedure is known as a colectomy. Depending on the extent of the cancer and the surgery’s impact on the colon, a temporary or permanent colostomy may be necessary.
Chemotherapy: After surgery, chemotherapy is usually recommended to kill any remaining cancer cells that can’t be seen, reducing the risk of cancer recurrence. Chemotherapy can be administered before surgery (neoadjuvant chemotherapy) to shrink tumors or after surgery (adjuvant chemotherapy) to eliminate any residual cancer cells. The specific drugs and duration of treatment will depend on the individual case but typically involve several months of therapy.
Radiation Therapy: Although less common than in rectal cancer, radiation therapy is sometimes used in conjunction with chemotherapy for stage 3 colon cancer if the tumor is large or if there are concerns about cancer cells remaining after surgery. Radiation therapy involves targeting the affected area with high-energy rays to destroy cancer cells, which helps to reduce the risk of recurrence.
Targeted Therapy: For some patients, targeted therapies that focus on specific abnormalities within cancer cells may be an option. These drugs can block the growth and spread of cancer cells while limiting damage to normal cells. Whether targeted therapy is suitable depends on the genetic makeup of the tumor, which can be assessed through molecular testing.
Immunotherapy: In cases where colon cancer has specific genetic features that make it less likely to respond to traditional chemotherapies, immunotherapy might be recommended. This treatment option uses medicines that help your immune system recognize and attack cancer cells more effectively.
Clinical Trials: Participating in clinical trials can also be a valuable treatment avenue for stage 3 colon cancer patients. Clinical trials offer access to new therapies and drugs not yet available on the market and can be discussed with your healthcare provider.
Throughout this journey, it’s crucial to maintain open and continuous communication with a team of healthcare professionals, including oncologists, surgeons, dietitians, and support staff, who can provide guidance tailored to your specific condition. They will help navigate through these options, manage side effects efficiently, and adjust treatments as needed based on how your cancer responds.
By understanding each treatment option available for stage 3 colon cancer, patients and their families can make more informed decisions about their health care strategy. It’s essential to weigh each treatment’s benefits against potential risks and side effects by discussing these aspects thoroughly with your oncology team.
3. Factors Influencing Prognosis and Survival Rates
The prognosis and survival rates for Stage 3 colon cancer can vary significantly, influenced by a variety of factors. Understanding these can help patients and their families better prepare for the treatment journey and potentially improve outcomes.
Firstly, the extent of the cancer spread is crucial. Stage 3 colon cancer is characterized by cancer that has spread beyond the original tumor site to nearby lymph nodes but not to distant organs. Within Stage 3, there are sub-stages – 3A, 3B, and 3C – each representing a greater extent of lymph node involvement and generally a poorer prognosis as the sub-stage progresses.
Another significant factor is the patient’s overall health and age at diagnosis. Younger patients often have better survival rates due to their generally better overall health and higher resilience in handling aggressive treatments like chemotherapy. Conversely, older patients or those with significant comorbidities such as diabetes or heart disease may face a tougher prognosis.
The molecular characteristics of the cancer itself also play a role. For instance, tumors with certain genetic mutations or markers may respond differently to treatments. Testing for these markers can sometimes lead to more personalized treatment approaches, which might improve prognosis. For example, tumors that are MSI-High (microsatellite instability-high) have been found to respond better to immunotherapy, an emerging treatment modality.
Treatment response is another critical factor. How well a patient’s cancer responds to initial treatment such as surgery and chemotherapy significantly affects survival outcomes. Complete surgical removal of the tumor and effective lymph node clearance without postoperative complications tends to be associated with a better prognosis. Additionally, patients who respond well to chemotherapy usually have a better outlook than those who do not.
Furthermore, lifestyle factors can also influence survival rates. Patients who maintain a healthy diet, engage in regular physical activity, and do not smoke typically experience better overall health which can support them through their cancer treatment. Studies have shown that obesity and smoking are linked with poorer outcomes in colon of cancer patients.
Regular follow-up care post-treatment is crucial in managing Stage 3 colon cancer effectively. This includes regular check-ups, scans, blood tests, and sometimes additional adjuvant therapies that can help detect any recurrence early and manage it promptly.
Finally, psychosocial factors also significantly impact survival rates. Support from family, friends, healthcare professionals, and even support groups can provide emotional sustenance that is critical during treatment. Mental health influences physical health; hence managing stress, anxiety, and depression through counseling or other therapeutic approaches can contribute positively to a patient’s overall wellbeing and potentially their prognosis.
In summary, while Stage 3 colon cancer presents significant challenges, multiple factors influence its prognosis and survival rates. Understanding these can help in tailoring treatment approaches and supporting strategies that enhance both the quality of life and survival chances for patients.
4. Advances in Medical Research and Emerging Therapies
The landscape of colon cancer treatment is continuously evolving, with significant advances in medical research leading to the development of new and emerging therapies that offer hope and improved outcomes for patients diagnosed with stage 3 colon cancer. These advancements not only aim to enhance the efficacy of existing treatments but also to provide options that are more targeted and less toxic.
One of the most promising areas of research is immunotherapy, which utilizes the body’s immune system to fight cancer. Unlike chemotherapy, which indiscriminately kills rapidly dividing cells, immunotherapy works by helping the immune system recognize and destroy cancer cells specifically. For stage 3 colon cancer, immunotherapies such as checkpoint inhibitors have shown potential. These drugs work by blocking proteins that prevent immune cells from attacking cancer cells, thereby enabling a stronger immune response against the tumor.
Another exciting development is targeted therapy, which focuses on specific molecules and signaling pathways that are crucial for the growth and survival of cancer cells. By targeting these pathways, these therapies can block the growth and spread of cancer cells while sparing healthy cells, leading to fewer side effects compared to traditional chemotherapy. Drugs such as bevacizumab (Avastin) and cetuximab (Erbitux) have been used in treating stage 3 colon cancer, particularly when the cancer has high levels of specific proteins that these drugs target.
Additionally, advances in genetic and molecular profiling of tumors are paving the way for personalized medicine in colon cancer treatment. By analyzing the genetic makeup of a patient’s tumor, oncologists can identify unique biomarkers and predict which treatments will be most effective. This approach ensures that patients receive the most appropriate therapies tailored to their specific cancer type, potentially improving outcomes and reducing unnecessary side effects.
Research is also being conducted on vaccine therapy for colon cancer. Unlike traditional vaccines that prevent diseases, cancer vaccines are designed to be administered after the diagnosis. These vaccines aim to boost the immune system’s response to cancer by teaching it to recognize and attack specific cancer-related antigens. While still largely experimental, vaccine therapy represents a novel approach that could complement existing treatments for stage 3 colon cancer.
Lastly, the role of microRNA (miRNA) in colon cancer progression and treatment resistance is another area under investigation. miRNAs are small non-coding RNA molecules involved in regulating gene expression. Studies suggest that altering miRNA expression in cancer cells can affect their proliferation, apoptosis (programmed cell death), and sensitivity to chemotherapy. Therapies designed to modulate miRNAs could potentially reverse resistance to chemotherapy and improve treatment outcomes for patients with advanced-stage colon cancer.
These advances in medical research demonstrate a robust commitment to finding more effective and less harmful treatment options for stage 3 colon cancer. While many of these therapies are still under clinical trials, their potential to significantly improve patient prognosis offers hope for those affected by this challenging disease.
5. Living with Stage 3 Colon Cancer: Lifestyle Changes and Support Systems
Living with stage 3 colon cancer can be profoundly challenging, but incorporating certain lifestyle changes and leveraging support systems can significantly enhance quality of life and potentially impact the effectiveness of treatment. Patients and their families often find that addressing the physical, emotional, and social aspects of cancer care is crucial for navigating this journey.
Dietary Adjustments: Nutrition plays a pivotal role in managing colon cancer. A diet rich in fruits, vegetables, whole grains, and lean proteins can help strengthen the body’s defenses and support recovery during treatments like chemotherapy and radiation. It’s important to consult with a dietitian who specializes in cancer care to tailor dietary plans that meet individual nutritional needs and manage side effects related to treatment.
Physical Activity: Regular exercise is another cornerstone of living well with colon cancer. Activities such as walking, yoga, and light strength training can improve physical function, decrease fatigue, and elevate mood. However, it’s essential to discuss and design an exercise plan with healthcare providers to ensure all activities are safe and appropriately matched to one’s health status.
Emotional and Psychological Support: The emotional burden of cancer can be as challenging as the physical aspects. Engaging with psychologists or counselors who specialize in oncology can provide strategies to manage stress, anxiety, and depression. Many find solace in support groups where sharing experiences with others facing similar challenges offers comfort and camaraderie.
Integrative Therapies: Complementary therapies such as meditation, acupuncture, massage therapy, and biofeedback can help manage symptoms and improve overall well-being. These therapies should complement conventional treatments; discussing them with the healthcare team ensures they are delivered safely and effectively.
Social Support Networks: Strong support from family, friends, community resources, and cancer support organizations can provide a substantial emotional lift and practical help. Tasks that were once simple, such as household chores or running errands, can become daunting during treatment. Help from loved ones can relieve these burdens, allowing the patient to focus more on recovery.
Educational Resources: Understanding the disease and its treatment options can empower patients and reduce uncertainties. Healthcare providers can recommend reliable sources of information that provide insights into stage 3 colon cancer treatments, side effects, and new research findings.
Regular Medical Care: Keeping up with regular check-ups, treatment sessions, and follow-up care is crucial for managing stage 3 colon cancer effectively. These visits are not only for administering treatment but also for monitoring progress, managing side effects, and making adjustments to the treatment plan as necessary.
Navigating life with stage 3 colon cancer involves a comprehensive approach that includes medical treatment along with lifestyle adjustments and robust support systems. Each aspect of care plays a unique role in maintaining health and well-being. By actively participating in their care plan, individuals diagnosed with stage 3 colon cancer can better manage their symptoms and lead a fulfilling life despite the challenges posed by the disease.
Conclusion:
Facing Stage 3 colon cancer requires a multi-faceted approach that involves understanding the medical aspects of the disease, as well as incorporating lifestyle changes and psychological support. With advances in medical science offering new therapies and treatments that increase survival rates and improve quality of life, there is hope for patients navigating this challenging stage of cancer. It’s imperative for patients and their families to stay informed, maintain open communication with healthcare providers, and access supportive resources to manage the impact of colon cancer effectively.
