title: Understanding the Pain Associated with Colon Cancer: A Comprehensive Guide
1. Introduction to Colon Cancer and Its Common Symptoms
2. The Nature of Pain in Colon Cancer: What Patients Experience
3. Factors Influencing Pain Levels in Colon Cancer Patients
4. Managing Pain: Treatment Options and Supportive Care for Colon Cancer
5. When to Seek Help: Recognizing Pain as a Symptom of Progression or Complications
Introduction: Colon cancer is a serious and potentially life-threatening condition that affects thousands of people each year. Understanding the pain associated with this disease is crucial for patients, caregivers, and healthcare providers alike. This comprehensive guide aims to delve into the various aspects of pain experienced by colon cancer patients, exploring its causes, progression, and effective management strategies. By equipping readers with this knowledge, we aim to empower them to better manage symptoms and improve the quality of life for those affected.
1. The Nature of Pain in Colon Cancer: What Patients Experience
Pain is a common and significant symptom for many individuals diagnosed with colon cancer. This type of pain can vary greatly in character and intensity, depending on several factors such as the stage of the cancer, its location within the colon, and how much it has spread to other areas of the body. Understanding the specific nature of pain that colon cancer patients experience is crucial for effective management and providing appropriate support.
Initially, the pain may be vague and intermittent, often described as cramping or discomfort in the abdomen. This can sometimes be mistaken for common digestive complaints. As the tumor grows, it can obstruct part of the colon, leading to more pronounced and constant pain. The sensation might feel like a deep ache or pressure in the lower abdomen or pelvic area. Some patients report experiencing sharp, stabbing pains that come and go in waves.
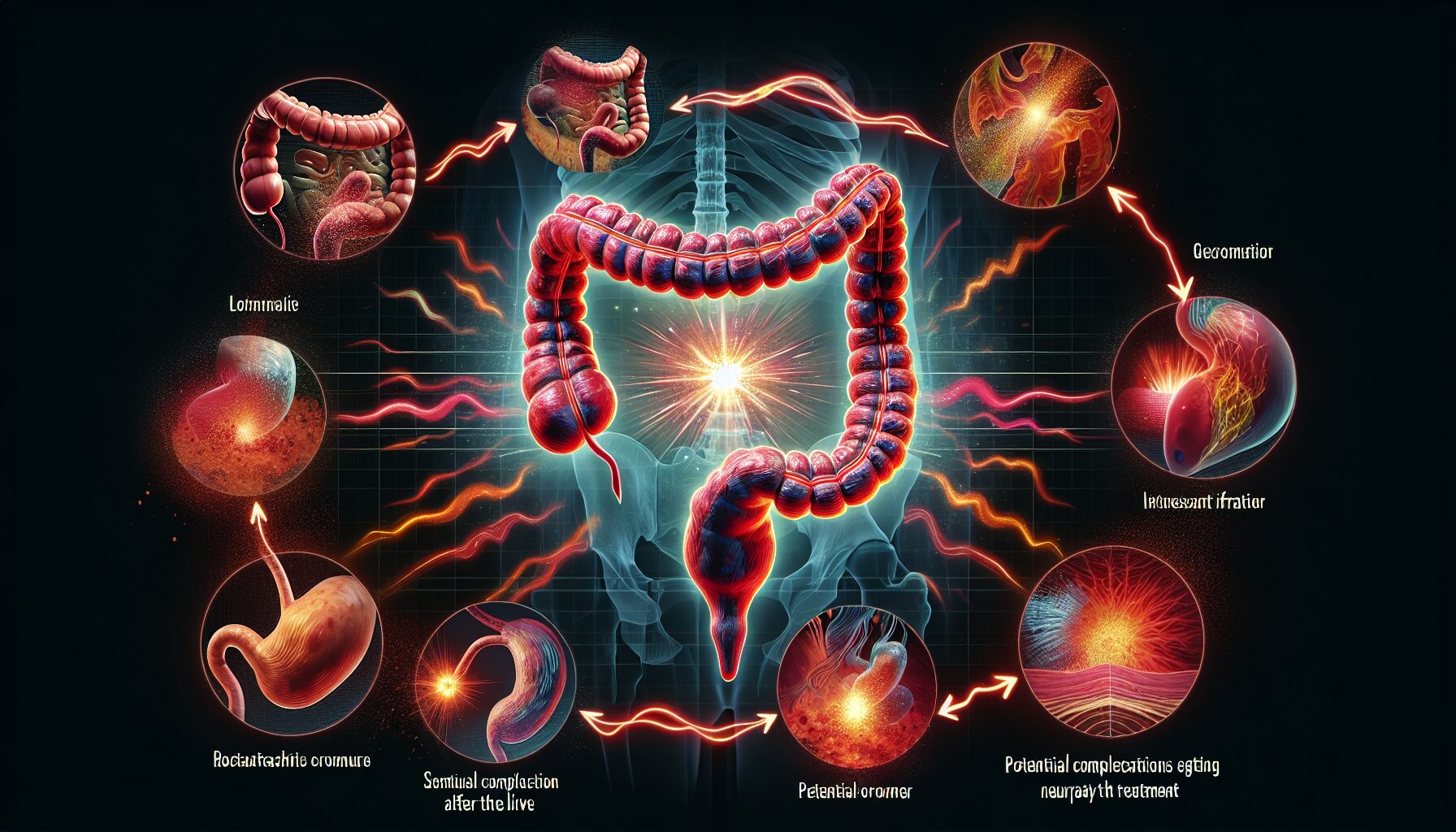
Furthermore, if the cancer spreads to surrounding tissues or organs, the character of the pain can change and intensify. For instance, if it invades the bladder or rectum, it may cause painful sensations during urination or bowel movements. Metastasis to the liver or other distant organs can also lead to additional pain and discomfort in other parts of the body.
The presence of a tumor can irritate the lining of the abdomen, leading to a condition known as peritoneal irritation. Patients with this condition often experience a sharp, piercing pain that can be exacerbated by movement or even breathing deeply. Additionally, as cancer progresses, it can lead to complications such as bowel perforation or blockages, each contributing to severe pain episodes.
Cancer treatments themselves, such as surgery, chemotherapy, or radiation therapy, can also introduce new types or intensities of pain. Post-operative pain is common and expected after surgical interventions to remove tumors or affected parts of the colon. Chemotherapy and radiation might cause painful side effects including neuropathy (nerve damage) which manifests as tingling, burning, or shooting pains primarily in the hands and feet.
It’s important for patients and caregivers to understand that experiencing pain does not always correlate directly with the progression of cancer. Various non-cancer related factors such as muscle strains from decreased activity levels, constipation commonly caused by medication, or even stress and anxiety can exacerbate feelings of pain.
For many patients dealing with colon cancer, pain is a persistent issue that affects quality of life significantly. Being open about their pain levels with healthcare providers ensures that these symptoms are appropriately addressed. Effective pain management is pivotal not only for improving quality of life but also for enhancing the effectiveness of other treatments by enabling patients to maintain better overall health and activity levels. Understanding what types of pain are typical among colon cancer patients allows caregivers and medical teams to better anticipate and manage these challenges as they arise during treatment.
2. The Nature of Pain in Colon Cancer: What Patients Experience
Pain associated with colon cancer can vary significantly among patients, both in terms of intensity and the way it is experienced. This variability is largely influenced by the location of the tumor, its size, and the extent to which it has spread. Understanding the nature of this pain can help patients and caregivers better prepare for the challenges ahead.
In the early stages of colon cancer, patients may experience minimal or no pain. However, as the disease progresses, pain can become a more prominent symptom. The pain often starts as a mild discomfort or cramping in the abdomen, which can be easily mistaken for digestive issues or other common conditions. As the tumor grows, it can obstruct parts of the colon, leading to increased pressure and pain. This obstruction can also cause swelling and build-up of gas and stool, which exacerbates discomfort.
Additionally, if the cancer spreads beyond the colon to nearby organs or the peritoneum (the lining inside the abdomen), it can cause sharp, localized pain or a dull widespread ache. Metastasis to other parts of the body, such as the liver or lungs, might not directly affect abdominal pain but can contribute to overall discomfort and ill health.
Another source of pain in colon cancer patients is related to treatment procedures. Surgical interventions, while necessary to remove tumors, can lead to postoperative pain and sensitivity around the incision sites. Chemotherapy and radiation therapy, common treatments for colon cancer, also have side effects that can cause painful conditions like mouth sores, neuropathy (nerve damage), and skin irritation.
For some patients, the psychological burden of dealing with cancer can also manifest physically as pain. Anxiety and depression associated with a cancer diagnosis can increase the body’s sensitivity to pain and make existing pain feel worse.
It is important for patients to communicate their pain accurately and regularly to their healthcare providers. Keeping a “pain diary” that details when the pain occurs, its intensity, what seems to trigger it, and what alleviates it can be particularly useful. This record helps in tailoring treatment plans that address not only the cancer itself but also enhance the patient’s quality of life by managing symptoms effectively.
Understanding and managing pain in colon “cancer requires an integrated approach that considers both physical and emotional factors. By acknowledging and addressing each aspect of pain, healthcare providers can offer more comprehensive care that supports both the physical health and mental well-being of their patients.
3. Factors Influicing Pain Levels in Colon Cancer Patients
The experience of pain in colon cancer patients can vary widely, influenced by a range of factors that can either intensify or mitigate the discomfort. Understanding these factors is crucial for patients and caregivers alike, as it helps in managing expectations and tailoring pain management strategies effectively.
One primary factor is the stage of the cancer. In early stages, colon cancer might not cause any pain. However, as the disease progresses, it can lead to more significant pain symptoms. Advanced colon cancer often involves the tumor growing through the bowel wall or spreading to other organs, which significantly increases pain levels.
The location of the tumor also plays a critical role in the type of pain experienced. Tumors located near nerve centers or those that obstruct parts of the bowel can cause severe pain and discomfort. For instance, a tumor in the lower colon or rectum is likely to cause more pain due to its proximity to several nerves and muscles involved in bowel movements and sitting.
Another significant factor is the individual’s overall health and body response. Patients with a higher overall body inflammation or those who have other underlying conditions like irritable bowel syndrome (IBS) or previous abdominal surgeries may experience heightened pain. This is because their body’s threshold for pain may already be lowered, making them more sensitive to new pain sources.
Treatment methods themselves can also influence pain levels. Surgical procedures, while often necessary to remove tumors, can lead to post-operative pain and complications that add to discomfort. Chemotherapy and radiation therapy, common treatments for colon cancer, have side effects such as nausea, vomiting, and mucositis (inflammation of the mucous membranes lining the digestive tract), which can exacerbate feelings of discomfort and pain.
Psychological factors are equally influential. The emotional stress associated with a cancer diagnosis can heighten one’s sensitivity to pain. Anxiety and depression are common among cancer patients and can alter the perception of pain. Managing these psychological aspects through counseling or therapy can be an essential part of comprehensive pain management.
Lastly, lifestyle factors such as diet and physical activity play roles in managing pain levels. A diet that exacerbates bowel discomfort or causes constipation can increase pain for colon cancer patients. Conversely, a well-balanced diet rich in fiber can help maintain bowel regularity and reduce discomfort. Regular gentle exercise has been shown to help reduce inflammation and improve mood, which might indirectly help manage pain better.
Understanding these factors allows patients and healthcare providers to adopt a more personalized approach to managing pain associated with colon cancer. By considering how each element contributes to pain levels, better strategies for relief and quality of life improvement can be implemented.
4. Managing Pain: Treatment Options and Supportive Care for Colon Cancer
Managing pain effectively is crucial for improving the quality of life in individuals diagnosed with colon cancer. Pain management strategies encompass a range of treatments from medications to supportive therapies, aiming to address both the physical and emotional aspects of pain.
Medication is often the first line of defense. Depending on the intensity and nature of the pain, doctors may prescribe various types of pain relievers. For mild to moderate pain, over-the-counter drugs such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen may be sufficient. For more severe pain, especially pain caused by tumor growth or metastasis, stronger opioids like morphine or fentanyl might be necessary. It’s important for patients to communicate openly with their healthcare providers about the effectiveness of their pain medication and any side effects they may experience.
In addition to pharmaceutical approaches, there are numerous non-medical treatments that can help manage pain. Physical therapy can be particularly beneficial in alleviating discomfort and improving physical function. A physical therapist might employ techniques such as massage, heat treatment, or specific exercises to enhance mobility and reduce stiffness or soreness.
Another significant aspect of pain management is psychological support. Chronic pain can lead to significant stress, anxiety, and depression. Counseling or therapy sessions with a psychologist can help patients develop coping strategies to deal with the emotional toll of cancer. Cognitive-behavioral therapy (CBT), in particular, has been shown to be effective in managing chronic pain by changing the way patients perceive and react to their pain.
Nutritional support also plays a key role in managing symptoms and improving overall well-being. A dietitian specializing in cancer care can provide personalized advice on choosing foods that are easy to digest, nutritious, and capable of boosting energy levels. Proper nutrition can help maintain body strength and reduce treatment side-effects, which indirectly helps in managing pain.
Integrative therapies such as acupuncture, yoga, and meditation have also gained popularity for their role in pain relief. Acupuncture involves inserting thin needles into specific points on the body, which is believed to trigger the release of endorphins and other natural body painkillers. Yoga combines physical postures, breathing exercises, and meditation to enhance physical flexibility, reduce tension, and promote relaxation. Meditation helps in focusing thoughts away from the pain and reducing anxiety.
Finally, social support from family, friends, support groups, or a community of fellow patients can provide emotional comfort and practical help. Sharing experiences with others who understand what it feels like to live with colon cancer can be incredibly reassuring and decrease feelings of isolation or despair.
In summary, managing colon cancer-related pain requires a comprehensive approach that includes both medical treatments and supportive care practices. By combining medication with physical therapy, psychological support, nutritional advice, integrative therapies, and social support, patients can achieve better control over their pain and significantly improve their quality of life during treatment and recovery.
5. When to Seek Help: Recognizing Pain as a Symptom of Progression or Complications
Experiencing pain can be a normal part of the journey for those battling colon cancer, but there are specific situations where pain might indicate a progression of the disease or the onset of complications. It is crucial for patients and caregivers to understand when to seek medical advice beyond routine check-ups.
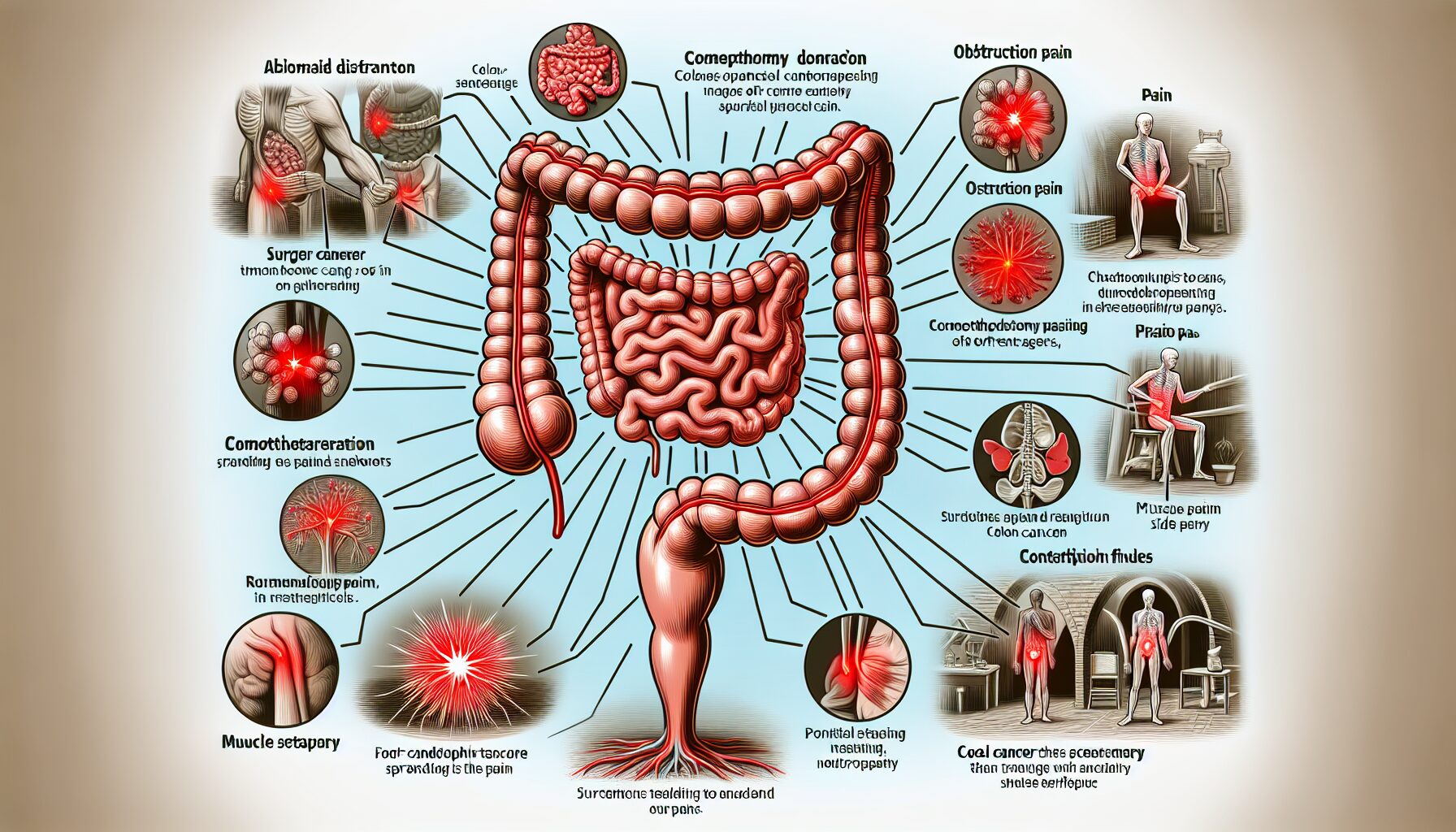
Firstly, a sudden increase in pain intensity or a change in the nature of the pain experienced can be a red flag. For example, if pain that was previously dull and manageable becomes sharp and severe, it may suggest complications such as a bowel obstruction or perforation, which require immediate medical attention. Similarly, pain that suddenly localizes to one specific area can also be indicative of tumor growth pressing on nerves or other organs.
Secondly, the development of new types of pain should prompt a consultation with a healthcare provider. If you begin to experience severe cramping, stabbing pains, or persistent aching that wasn’t present before, it could be a sign that the cancer is affecting new areas. This kind of pain might be accompanied by other worrying symptoms such as nausea, vomiting, or changes in bowel habits, which also need to be evaluated promptly.
Another critical indicator that warrants medical help is pain that does not respond to medications that previously proved effective. This resistance can be an indication that the cancer has progressed or that there is a new issue to address. Continuous pain that interferes with daily activities and reduces quality of life deserves reassessment of your pain management plan.
Additionally, any pain accompanied by other alarming symptoms such as rectal bleeding, significant weight loss, jaundice (yellowing of the skin and eyes), or an unexplained fever should immediately be reported. These symptoms could indicate severe complications like liver metastasis or infections that need rapid intervention.
It’s also important for patients receiving chemotherapy to report any new or worsening pain. Chemotherapy can lead to side effects like neuropathy (nerve damage) which manifests as tingling, numbness, or pain in the hands and feet. While this is often expected, excessive pain can indicate that adjustments need to be made to your treatment regimen.
For those managing chronic pain due to colon cancer, regular communication with your healthcare team is key. Keeping track of any changes in your pain’s characteristics (such as location, intensity, and what triggers or relieves it) can help your doctors make informed decisions about further diagnostic tests or adjustments in treatment necessary.
Remember, you know your body best. Any change in your usual pattern of pain should be taken seriously as it may provide crucial clues about your health status. Early intervention can significantly influence the outcome and management of colon cancer, so never hesitate to seek help if your pain pattern changes or becomes more difficult to control. Regular consultations with your healthcare team not only help manage physical symptoms but also provide support and reassurance during this challenging time.
Conclusion:
The journey through colon cancer is undoubtedly challenging, particularly when dealing with pain that often accompanies the disease. This guide has provided insights into understanding the different facets of pain related to colon cancer, from identifying its early signs to implementing effective management strategies. It’s essential for patients and their support systems to recognize when pain indicates a more serious complication and to seek timely medical intervention. With proper management and support, it is possible to enhance patient comfort and potentially improve outcomes in the battle against colon cancer.

GIPHY App Key not set. Please check settings