Title: Understanding Enlarged Prostate: Can It Go Back to Normal?
An enlarged prostate, also known as benign prostatic hyperplasia (BPH), is a common condition that affects many men as they age. This condition can lead to uncomfortable urinary symptoms, such as blocking the flow of urine out of the bladder and causing bladder, urinary tract, or kidney problems. The question that often arises is: Can an enlarged prostate go back to normal? This article delves into the nature of BPH, its causes, symptoms, treatment options, and whether it is possible for the prostate to return to its normal size.
Understanding Benign Prostatic Hyperplasia (BPH)
The prostate is a small gland located below the bladder and in front of the rectum. It surrounds the urethra, the tube through which urine exits the body. As men age, the prostate gland can enlarge, which is a natural part of aging. BPH is not cancerous and does not increase the risk of prostate cancer. However, it can significantly affect quality of life due to its impact on urinary functions.
Causes of Enlarged Prostate
The exact cause of BPH is not fully understood, but several factors are believed to play a role:
1. Aging: The likelihood of developing BPH increases with age. It rarely causes symptoms before age 40, but more than half of men in their 60s and up to 90% of men in their 70s and 80s have some symptoms of BPH.
2. Hormonal Changes: Changes in the balance of sex hormones as men grow older may cause prostate gland growth.
3. Family History: Having a blood relative with prostate problems may increase your risk.
4. Lifestyle Factors: Obesity, lack of physical activity, and certain dietary factors can contribute to BPH.

Symptoms of an Enlarged Prostate
The severity of symptoms varies among individuals but tends to gradually worsen over time. Common signs and symptoms include:
– Frequent or urgent need to urinate
– Increased frequency of urination at night (nocturia)
– Difficulty starting urination
– Weak urine stream or a stream that stops and starts
– Dribbling at the end of urination
– Inability to completely empty the bladder
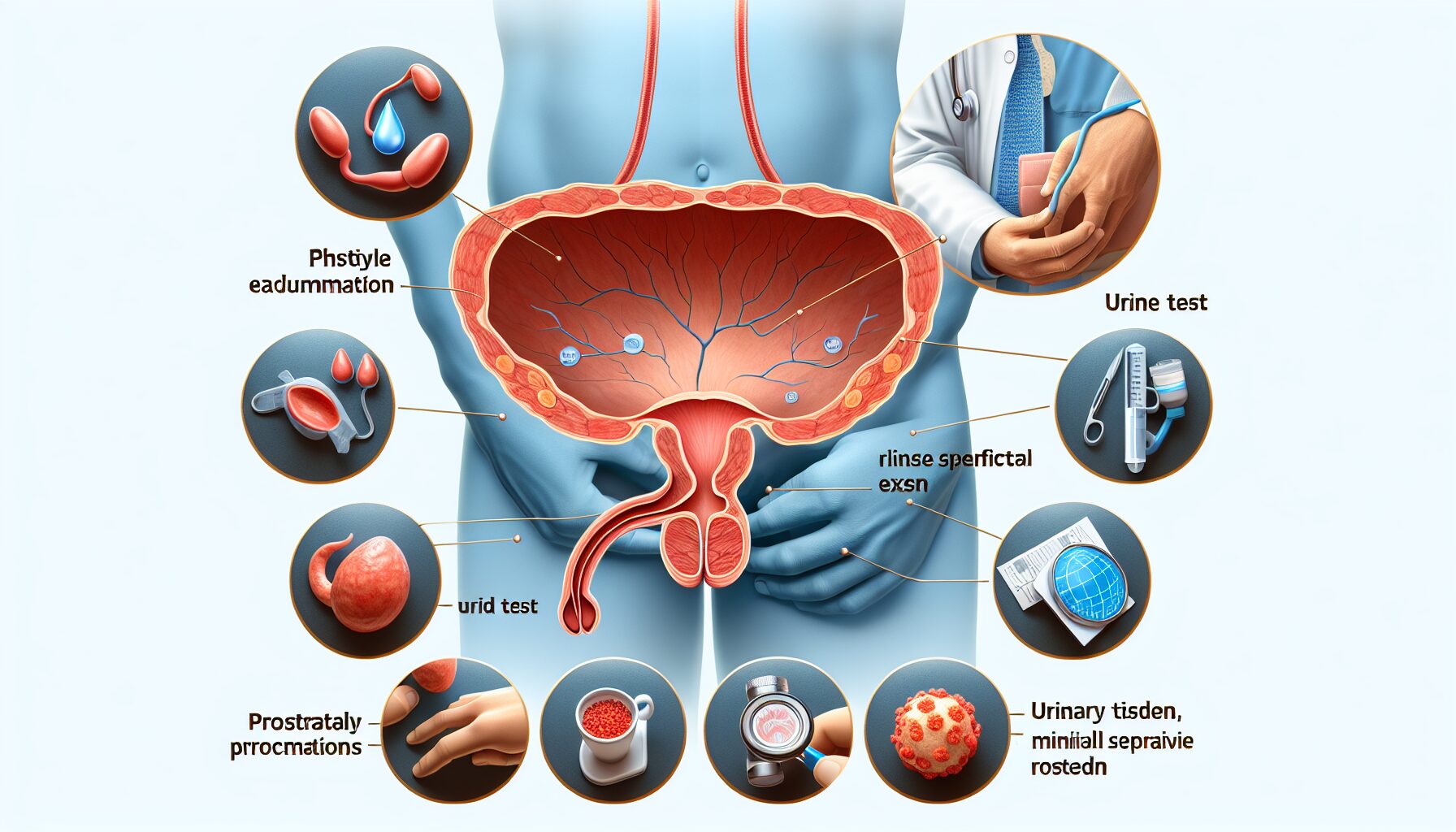
Diagnosis
To diagnose BPH, a healthcare provider will typically perform a physical examination and ask about symptoms. Tests may include:
– Digital Rectal Exam (DRE): To estimate the size of the prostate.
– Urine Test: To check for infection or other conditions that can cause similar symptoms.
– Blood Test: To check for kidney problems.
– Prostate-Specific Antigen (PSA) Test: While high PSA levels can indicate an enlarged prostate, they could also be a sign of prostate cancer.
– Urinary Flow Test: To measure strength and amount of urine flow.
– Postvoid Residual Volume Test: To determine if you can empty your bladder completely.
Treatment Options
Treatment for BPH depends on the severity of symptoms, size of the prostate, age, overall health, and patient preference. Options include lifestyle changes, medications, minimally invasive procedures, and surgery.
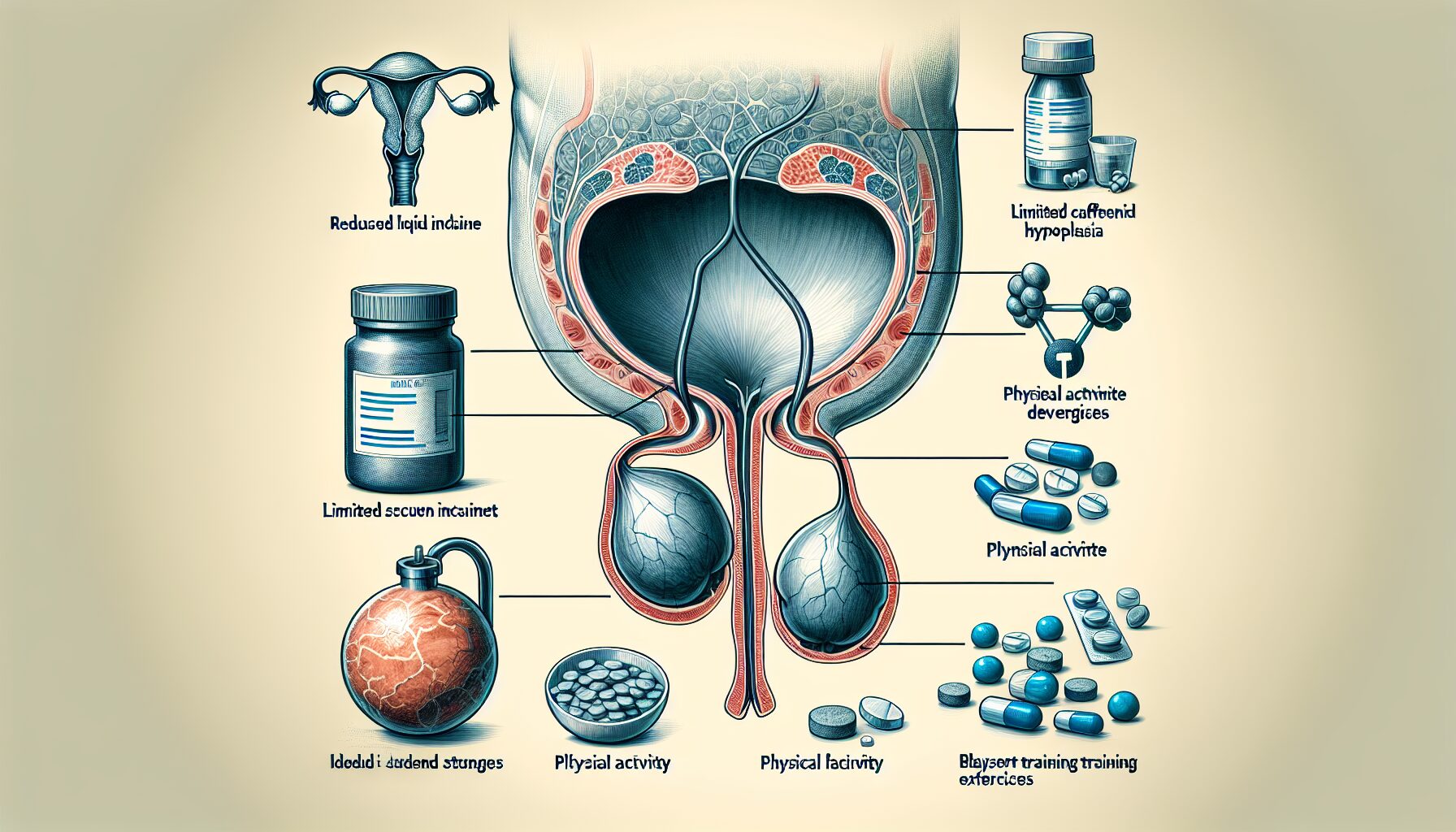
# Lifestyle Changes
For mild symptoms, simple lifestyle adjustments may help:
– Reducing liquid intake in the evening
– Limiting caffeine and alcohol
– Regular physical activity
– Practicing bladder training exercises
# Medications
Several medications can help manage BPH:
1. Alpha Blockers: These relax muscle fibers in the prostate and bladder neck to make urination easier.
2. 5-Alpha Reductase Inhibitors: These medications shrink the prostate by preventing hormonal changes that cause growth.
3. Combination Therapy: Sometimes using both alpha blockers and 5-alpha reductase inhibitors together can be more effective.
4. Tadalafil (Cialis): Typically used for erectile dysfunction, this medication can also treat BPH.
# Minimally Invasive Procedures
If medications are ineffective or cause side effects, minimally invasive treatments might be an option:
1. Transurethral Microwave Therapy (TUMT): Uses microwave energy to destroy excess prostate tissue.
2. Transurethral Needle Ablation (TUNA): Uses radio waves to heat and destroy part of the prostate tissue.
3. Water-Induced Thermotherapy: Uses heated water to reduce prostate size.
# Surgical Options
For severe cases or when other treatments fail, surgery may be necessary:
1. Transurethral Resection of the Prostate (TURP): The most common surgery for BPH; removes part of the prostate tissue.
2. Laser Surgery: Removes overgrown tissue using concentrated light beams.
3. Open Prostatectomy: An option when there is a very large prostate or complications such as bladder damage.
Can an Enlarged Prostate Go Back to Normal?
While treatment can significantly reduce symptoms and improve quality of life, whether an enlarged prostate can go back to “normal” depends on various factors:
1. Medications: 5-alpha reductase inhibitors can shrink the prostate by about 20% over time but do not return it entirely to its original size.
2. Lifestyle Changes: While helpful in managing symptoms, lifestyle changes alone are unlikely to reverse enlargement.
3. Surgical Interventions: Procedures like TURP or laser surgery remove excess tissue but do not prevent future growth.
In summary, while complete normalization may not be feasible for everyone, treatments can effectively manage symptoms and reduce prostate size significantly.
Conclusion
An enlarged prostate is a common issue that many men face as they age. While it may not be possible for the prostate to return entirely to its original size naturally or through treatment alone, various medical interventions can significantly alleviate symptoms and improve quality of life. If you experience any signs or symptoms associated with BPH, consult with a healthcare provider for an accurate diagnosis and appropriate treatment plan tailored to your needs.
